Cord Blood Collection Practices
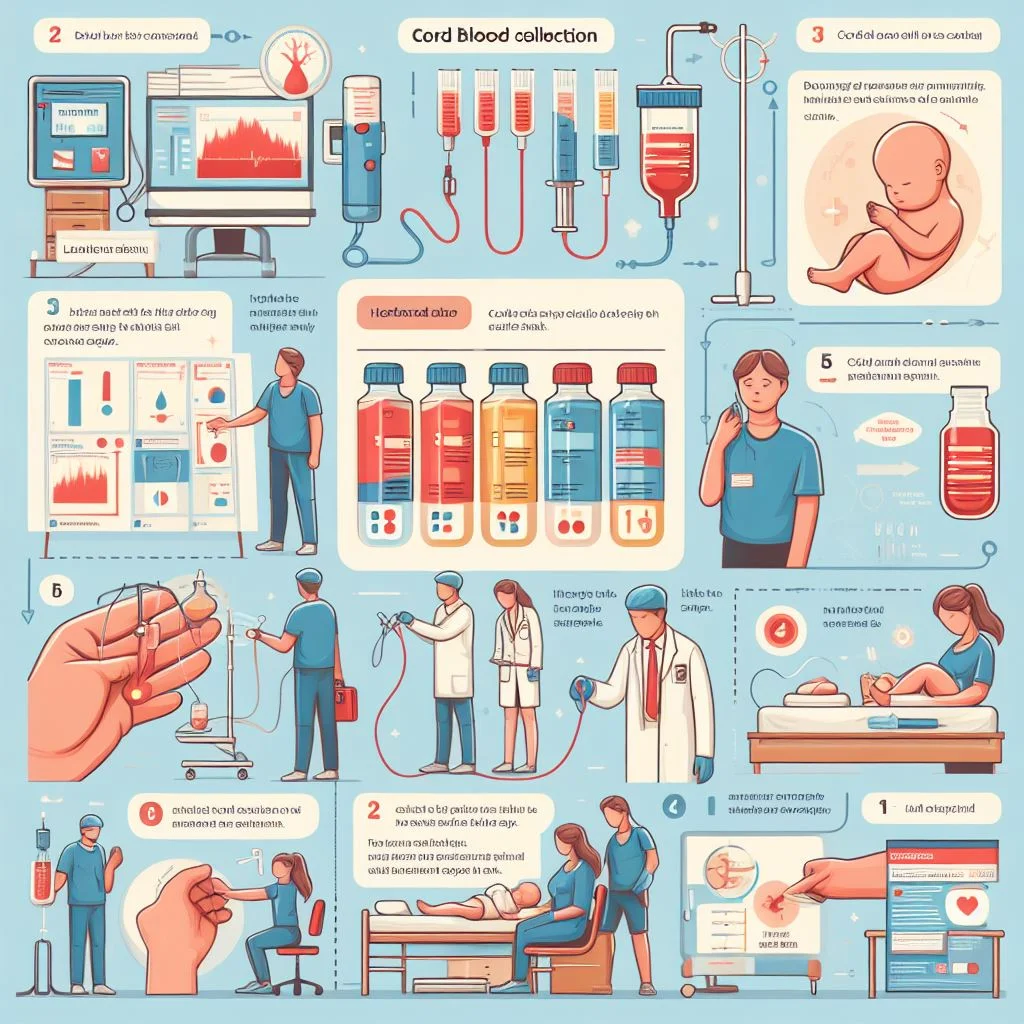
How is cord blood collected?
Collecting cord blood poses no health risk to the mother and infant donor. The cord blood is collected after delivery and would normally be discarded. The cord blood is stored only with the mother’s signed consent, and no collection is made if there are any complications during delivery.
After the baby’s birth, the umbilical cord is clamped, breaking the link between the baby and the placenta. Trained staff drains the blood from the umbilical cord and placenta. Methods vary somewhat at different hospitals but the idea remains the same. The blood is usually collected using a needle to draw the blood into a blood bag. The collection usually takes ten minutes or less.
Depending upon the type of delivery (e.g. Vaginal Delivery or Cesarean Section), the collection method is determined. During the process mother’s blood is collected first.
Collecting The Mother’s Blood: Perform a venipuncture to collect the mother’s blood. Both the red top and lavender top tubes should be filled and labeled with the mother’s name, SS# and date. This venipuncture can be performed prior to delivery and ideally should be done at the same time as the admission blood draw.
Collection of the cord blood takes place immediately after birth in both vaginal and cesarean (c-section) deliveries. It’s done using a specific kit that parents must order ahead of time from their chosen cord blood bank.
The umbilical chord is cut and clamped on both sides following a vaginal delivery. The cord blood is typically taken by a skilled obstetrician or nurse prior to placenta delivery. To collect the blood, one side of the umbilical cord is unclamped and a little tube is inserted into the umbilical vein. After blood has been collected from the cord, needles are placed on the side of the surface of the placenta that was connected to the fetus to collect more blood and cells from the large blood vessels that fed the fetus.
During cesarean births, cord blood collection is more complicated because the obstetrician’s primary focus in the operating room is tending to the surgical concerns of the mother. After the baby has been safely delivered and the mother’s uterus has been sutured, the cord blood can be collected. However, less cord blood is usually collected when delivery is by c-section. The amount collected is critical because the more blood collected, the more stem cells collected. If using the stem cells ever becomes necessary, having more to implant increases the chances of engraftment (successful transplantation).
Cord Blood Collection For Vaginal Delivery
The standard delivery practice of the institution must never be compromised for the collection of a cord blood sample. The prime concern is the safe delivery. Sample sterility is essential throughout the collection procedure, and every effort should be made to maximize the volume of cord blood collected. Umbilical cord is double clamped about one inch or less apart at the infant’s abdomen.
If the child is placed on the mother’s abdomen, then the cord should be clamped and cut prior to doing so. The umbilical cord can then be cut between the two clamps, and the baby removed. As soon as possible after the delivery and prior to the expulsion of the placenta, wipe the umbilical cord with 70% alcohol wipes followed by betadine at the needle insertion site (also called collection site) to ensure sterility. The needle insertion site should be just above the clamp that remains on the cord. By gently twisting and pulling on the cap, remove the protective needle cap at the end of the tubing. And then insert the blood collection bag needle into the umbilical cord at the prepared site and hold in place.
Allow as much blood to flow into the bag as possible. The collection normally takes about 3-5 minutes or sometimes even more. Aim for filling the bag until it as at least half full. A collection that is less than ¼ of the bag will make adequate transplantation questionable, so a good volume is always better. If the vein collapses, then it may be necessary to work your way up the cord using additional insertion sites. Be sure to cleanse each site with alcohol and betadine as with the first. Snap the blue plastic needle guard around the collection tubing, noting that the arrow should be pointing toward the needle end of the tubing. As the needle is withdrawn from the cord, slide the needle guard over the exposed needle until it locks in place.
After Collection:
- When collection is completed, “milk” the blood in the tubing down the bag.
- Cut off the protected needle and discard it in the appropriate sharps container.
- Clamp the collection tubing twice with the provided umbilical cord clamps.
- Invert the bag gently several times to thoroughly mix the cord blood and the CPD anticoagulant.
Cord Blood Collection For Cesarean Section
Prior to C-Section: Place the contents of the C-Section Adaptor Kit on the sterile field. These sterile items include a 16 gauge needle, a 33cm extension set and a male adaptor (with luer lock). Connect the needle and the adaptor to the extension set.
At Delivery: Deliver the infant per standard practice, double clamping the cord after delivery. Position the extension so that the adaptor extends off the sterile field. Insert the needle from the collection bag into the male adaptor at the non-sterile end of the extension set. Insert the extension set needle into the umbilical vein to initiate the collection. Allow as much blood to flow into the bag as possible. The collection normally takes about 3-5 minutes. Aim for filling the bag until it as at least half full. A collection that is less than ¼ of the bag will make adequate transplantation questionable.
After Collection: When collection is completed, “milk” the blood in the tubing down the bag. Cut off the protected needle and discard it in the appropriate sharps container. Clamp the collection tubing twice with the provided umbilical cord clamps.
Additional Notes: If the placenta is spontaneously expelled before the collection is complete, or in the case of a C-Section when the placenta is quickly removed, the above procedure can be continued (or initiated) after the expulsion of the placenta. Elevating the placenta will typically assist in higher volume collections. Be sure to access only the fetal side of the placenta.